How Your Condition Started
Understanding what’s happening in your body is the first step toward recovery. That’s why we’ve spent over 25 years researching the science behind your symptoms.
The Root Cause: A Brain Stuck in Survival Mode

Your brain is designed to protect you.
Your brain is designed to protect you. In dangerous situations, it activates survival mechanisms – like increasing your heart rate, boosting immunity, or shutting down digestion. This response is led by two powerful brain regions:
- The amygdala, which detects threats
- The insula, which monitors the body’s internal signals and evaluates how serious those signals are
Usually, once the threat passes, the brain calms back down. But in some people, following a major stressor – such as a viral infection, physical injury, toxic exposure, or emotional trauma – this system becomes stuck in high alert. This is not your fault. It happens unconsciously, and it can happen to anyone.
Click on the numbers to find out more.
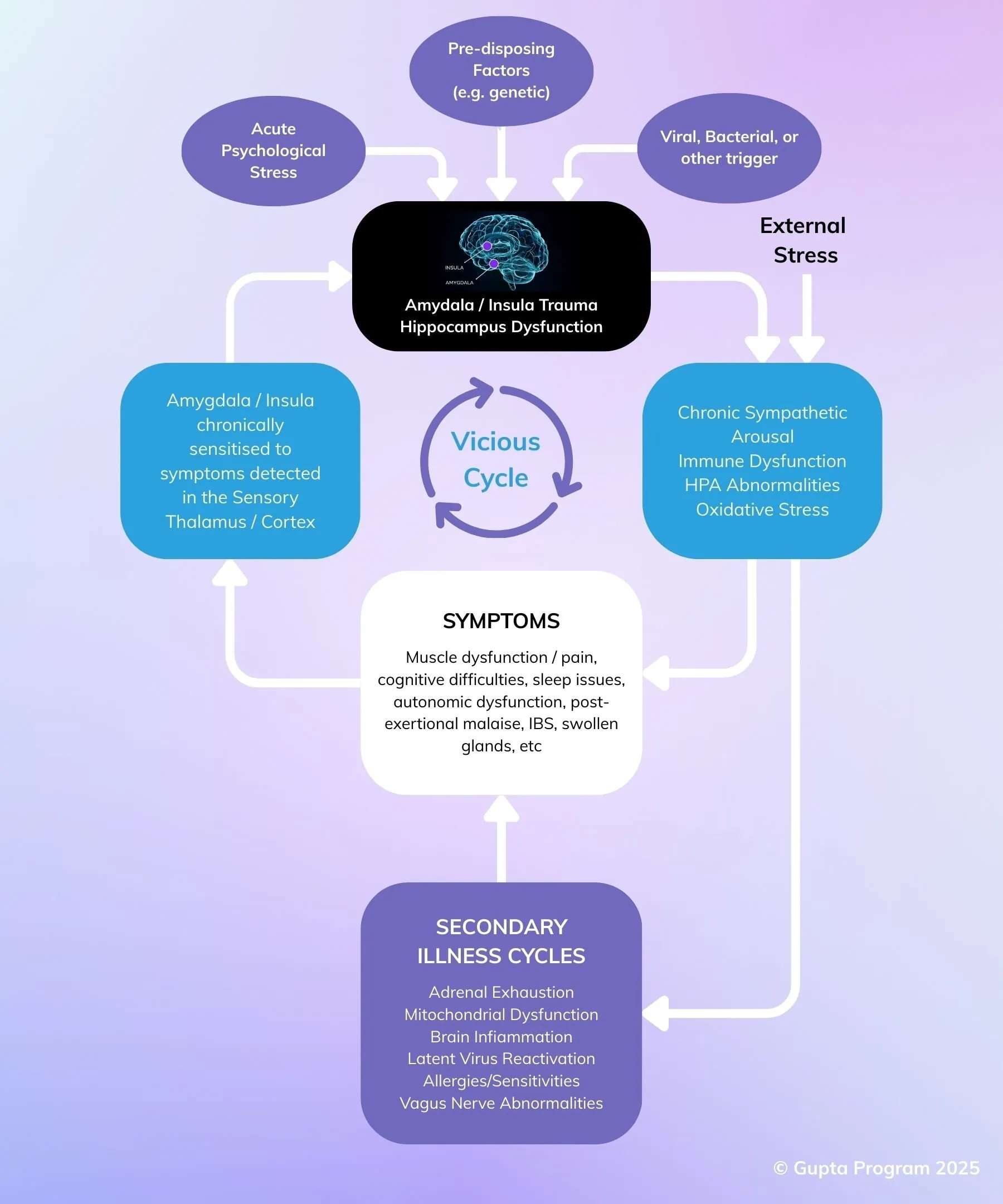
1. Why these conditions start
Some people have nervous systems that are naturally more sensitive — due to genetics, early experiences, or long-term stress.
On their own, these don’t cause illness, but they can make the body more reactive to stress.
A triggering event (like a virus, trauma, or toxic exposure) can then push the system past its tipping point.
2. What happens in the brain
When a major stressor hits, the brain’s protective systems — especially the amygdala and insula — go into high alert.
These areas can become “trained” to overreact to normal signals like pain or fatigue.
This response is automatic, not your fault, and completely outside of conscious control.
3. Chronic stimulation of the arousal system
With the brain stuck in protection mode, stress pathways stay switched on — flooding the body with stress hormones and disrupting sleep, mood, immunity, and energy levels.
This creates a whole-body ripple effect that feels very physical — because it is.
4. Symptoms begin
As stress systems stay active, real symptoms appear: exhaustion, brain fog, gut issues, pain, and more.
These aren’t imagined — they’re the body reacting to prolonged overload.
It can feel complex and overwhelming, but there is a pattern underneath it all.
5. Secondary illness cycles
The body becomes more sensitive over time, leading to more symptoms: disrupted sleep, chemical sensitivities, increased pain, and burnout.
These aren’t new illnesses — they’re part of the same overstimulated system looping on itself.
6. The brain detects symptoms
Once symptoms start, the brain focuses on them closely — scanning for more danger.
It begins misreading even normal body signals as signs of threat, keeping you stuck in a reactive state.
This is where hyper-awareness of symptoms can develop.
7. The alarm is re-triggered and the cycle restarts
When the brain detects symptoms, it reactivates the stress response — like hitting replay on the same loop.
The body stays on edge, and symptoms continue or flare up unexpectedly.
This explains the unpredictable, exhausting nature of many chronic conditions.
1. Why these conditions start
Some people are more likely to develop conditions like ME/CFS, fibromyalgia, or long COVID because of certain background factors. These might include:
- Genetics (family history of similar conditions)
- Childhood adversity or trauma
- Highly sensitive nervous systems
- Long-term stress or burnout
- Environmental exposures
These don’t cause illness on their own – but they can make the brain and body more sensitive to stress, which sets the stage for illness if something tips the system too far.
Then comes a trigger.
For many people, symptoms begin after a specific event that overwhelms the nervous system. This can be:
- Emotional stress – like a breakup, loss, trauma, or burnout
- Physical stress – like a virus, surgery, injury, or toxic exposure
Examples of common triggers:
- ME/CFS often starts after a viral infection (like glandular fever)
- Fibromyalgia can follow an accident or chronic pain
- MCS or Mold Illness might begin after exposure to chemicals or mold
- IBS often follows food poisoning or gut-related stress
- Long COVID starts after a viral infection, but symptoms persist beyond the typical recovery window
In some cases, like Gulf War Syndrome, people experience a combination of physical and emotional stressors – like vaccines, chemical exposure, and combat stress – all at once.
Why this matters:
- Some people get sick suddenly. Others slowly wear down over time.
- Symptoms vary – but the underlying pattern in the brain and nervous system is often the same.
That’s why so many of these conditions overlap, and why similar tools can help people with different diagnoses recover.
2. What happens in the brain
When you go through something stressful – like a virus, an injury, or emotional trauma – your brain works hard to protect you. That’s its job. But sometimes, this protective response becomes overactive and overly sensitive.
Two key parts of the brain play a role here:
- The amygdala – acts like an internal alarm system, always scanning for danger
- The insula – helps the brain read signals from inside your body (like pain, fatigue, or tension)
If the stress is intense or ongoing, these parts of the brain can get “stuck” in high alert. They start to overreact to normal body signals, interpreting them as threats – even when there’s no actual danger anymore.
3. Chronic stimulation of the arousal system
Once the amygdala and insula become conditioned to stay in high alert, they continue to overstimulate the body’s stress systems – even when no real danger is present.
This constant activation affects multiple areas:
The HPA Axis (Stress Hormone System)
The brain keeps the hypothalamus and adrenal glands switched on, flooding the body with stress hormones like cortisol. Over time, this system wears down, making it harder for the body to handle stress or recover properly.
Brain Chemistry and Arousal
The amygdala continues to activate brain circuits, keeping the whole system stuck in a state of hyper-arousal. This can reduce important brain chemicals like serotonin and dopamine, which affects mood, motivation, and focus. It also disrupts calming mechanisms that would normally tell the brain and body it’s safe again.
Immune System Conditioning
The immune system may also become conditioned to overreact. This means it can start responding to everyday triggers as if they’re threats, causing chronic inflammation and neuroinflammation – a type of irritation in the brain itself.
Oxidative Stress and System-Wide Impact
The ongoing stress response can create oxidative stress – a form of internal wear and tear that affects cells throughout the body. The immune and hormone systems can become unbalanced, which affects everything from digestion to sleep to energy.
This non-stop “false alarm” leads to a wide range of symptoms. But importantly, many of the physical changes seen in the body are not the root cause – they’re the result of the brain being stuck in this overprotective state.
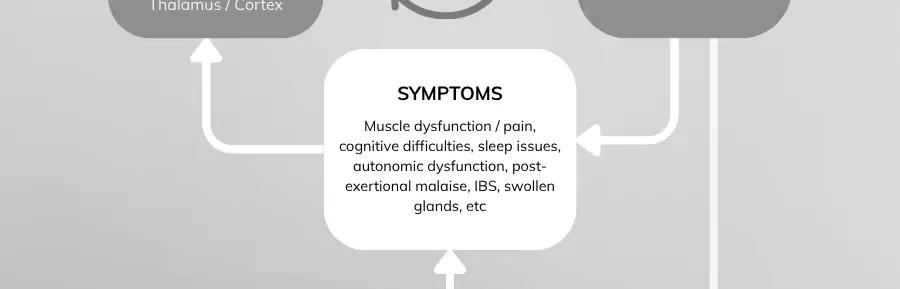
4. Symptoms begin
Once the brain and body stay stuck in high alert, real symptoms start to appear.
This is because the constant stimulation begins to wear down or disrupt key systems in the body:
- Some systems become less responsive over time (called “down-regulation”)
- Others become exhausted, like the adrenal glands
- The stress response can raise nitric oxide levels, which may damage cells and reduce energy production (mitochondrial dysfunction)
- The immune system becomes unbalanced, allowing dormant viruses — like HHV-6 — to become active again and increase symptom load
These physical effects can make the illness feel even more complex and overwhelming.
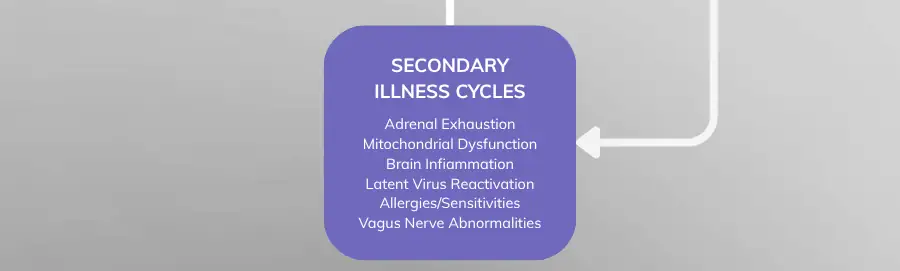
5. Secondary illness cycles
As this pattern continues, the body’s heightened sensitivity can lead to additional conditions. These are called secondary illness cycles, and they may include:
- Allergies or chemical sensitivities
- Disrupted sleep, especially a lack of restorative “delta” sleep
- Severe morning fatigue, even after a full night in bed
- Increased pain, particularly in conditions like fibromyalgia
These secondary issues don’t mean something new is “wrong” – they’re part of the same cycle of overstimulation. They show how far-reaching the impact of a hyper-alert brain can be.
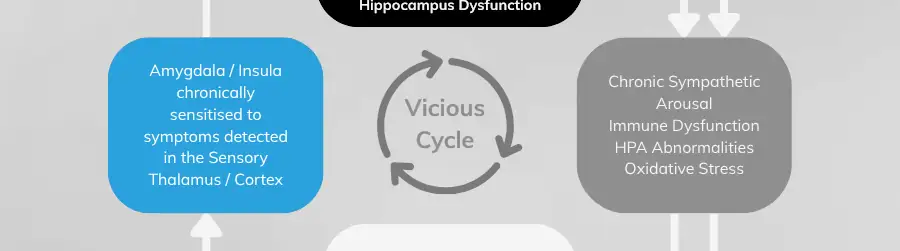
6. The brain detects symptoms
Once symptoms appear, the brain continues to notice and monitor them through areas like the sensory cortex, thalamus, and insula.
These regions are responsible for receiving signals from the body – pain, fatigue, discomfort – and deciding what they mean. But when the brain is already on high alert, it can start interpreting even normal signals as dangerous.
This misinterpretation keeps the nervous system in a reactive state, constantly scanning the body for signs of threat.

7. The alarm is re-triggered and the cycle restarts
The amygdala plays a key role in this final loop. When it detects symptoms — especially if the insula has labeled them as dangerous — it sends signals to re-activate the stress response.
This sends the body right back into the same state of over-arousal described earlier (Step 4), restarting the cycle.
This explains why symptoms don’t just stay the same — they often flare up, feel unpredictable, and continue even when everything else seems “normal.”
Over time, this feedback loop becomes deeply ingrained, and healing requires gently retraining these patterns.
What Influences the Severity of Symptoms?
Every person’s experience is different, depending on:
- How intense the original brain conditioning was
- What systems were affected at the time of the trigger
- When the conditioning occurred and how it evolved over time
For some, the loop is mild and symptoms improve with general lifestyle changes.
For others, the loop is deeply embedded, and symptoms are severe or long-lasting.

A Brain That Can Learn to Fear Can Also Learn to Heal
Your brain is incredibly adaptable – this ability is called neuroplasticity. With the right support, it can unlearn these harmful patterns and create new, healthy ones.
The Gupta Program uses gentle brain retraining, mindfulness, breathwork, and somatic practices to:
- Calm the limbic system
- Strengthen inhibitory feedback from the prefrontal cortex
- Rebuild emotional and physiological safety
- Support the nervous and immune systems in rebalancing

What the Research Shows
We now have peer-reviewed studies showing:
- Symptom reduction in ME/CFS, Fibromyalgia, and Long Covid
- Better outcomes than standard care in fatigue, mood, and quality of life
The brain can be reshaped, MRI studies show that practices like meditation can increase grey matter in key regulatory areas

Videos
The Evolutionary Background of Certain Chronic Conditions
The Insula & The Amygdala’s Relevance in Chronic Conditions
How the Condition Starts & Develops
The Vicious Cycle, How Chronic Conditions Perpetuate
Understanding is the first step toward healing. The fact that you're here, learning about your condition, shows incredible courage and commitment to your health.
Start your healing journey today with our 28-day free trial - no credit card needed

